In cell therapy development, a product’s potency – its biological activity – is a make-or-break attribute. Regulatory agencies consider potency a critical quality attribute (CQA) that must be measured for each lot to ensure the therapy will have its intended clinical effect. In FDA’s terms, potency is “the specific ability or capacity of the product to affect a given result”. In practice, this means developers need robust assays that quantify the therapy’s functional activity in alignment with its mechanism-of-action (MoA).
When designed and implemented well, potency assays defining a CQA do far more than satisfy a regulatory box-check – they can significantly accelerate development by guiding process decisions, ensuring consistent efficacy, and smoothing the path to approval. For clarity in this article, we define a “potency assay” as the validated, quantitative QC test used for lot release. This post explores why potency assays are so important in cell therapy development and how they can speed progress from bench to bedside.
Potency as a Cornerstone of Cell Therapy Quality
Potency testing for a CQA is expected to reflect the therapeutic MoA and ideally correlate with clinical outcomes. Unlike small molecules, cell therapies often work via complex, multifaceted biological mechanisms. A potency assay therefore provides direct evidence that the product is doing what it’s designed to do – for example, a CAR-T cell therapy’s potency assay might measure its ability to release certain key cytokines (e.g., IFN-γ).
Regulatory guidelines (FDA, EMA, USP, etc.) consistently emphasize that each cell therapy must have a quantitative potency assay relevant to its biology. Robust potency assays are fundamental to product characterization and quality control, informing us about identity, strength, and consistency. They are required for lot release testing and play a key role in comparability studies when process changes occur. In short, potency is the defining quality attribute that links a cell therapy’s lab measurements to its expected clinical benefit.
Regulators consequently demand convincing potency data throughout development. FDA’s guidance for cell and gene therapies expects manufacturers to develop and validate potency assays to support IND and BLA submissions. Every lot released must have the “specific ability or capacity to achieve the intended therapeutic effect”. This ensures patients consistently receive an active therapy. Developers who establish a meaningful potency assay early gain a critical gauge of efficacy for use in optimization and validation. As an Alliance for Regenerative Medicine briefing put it, regulators require potency measures for all biologics (including cell therapies) to guarantee consistent products for patients. Without a viable potency assay, a cell therapy cannot progress far in clinical development or reach the market.
Accelerating Development Through Early Potency Assay Selection
A perhaps less obvious benefit is how the right potency assay selection strategy can speed up development itself. By integrating potency testing early, developers can make data-driven decisions to optimize their product and process. However, selecting an assay that is more likely to be qualified for clinical and commercial use is very valuable—not all assays evaluated during preclinical stages will meet regulatory standards.
During process development, teams may compare different culture methods, gene modifications, or cell selection techniques by measuring their impact on potency. Yet many early-stage assays rely on biological materials (such as target cell lines) or research-grade instruments that can be difficult to qualify under GLP/GMP standards. Cell lines used in research settings often lack the chain-of-custody documentation needed for regulatory submission, and instruments common in R&D labs may not be appropriately validated for clinical use. If these issues aren’t addressed early, developers often face the need for bridging studies, requalification of reagents, or redevelopment of assays—causing costly delays.
Choosing an assay with a clear path to qualification can help avoid delays caused by regulatory concerns, reduce the need for expensive bridging work, and streamline tech transfer into manufacturing. It also allows developers to define acceptance and rejection criteria earlier in development and begin generating the data package needed for assay qualification—including measures of linearity, range, system suitability, accuracy, sensitivity, specificity, precision, and robustness. By anticipating these requirements, teams can design assays that scale smoothly and meet evolving regulatory expectations with fewer surprises.
Indeed, FDA and EMA guidelines recommend evaluating multiple potency assay approaches in early development because some assays may prove too variable or hard to validate. Identifying a workable potency assay (or assay matrix) in preclinical or Phase 1 stages helps avoid scrambling for a solution later on. FDA’s 2011 guidance advises sponsors to “initiate potency assay development by way of product characterization during preclinical and early clinical investigations to obtain as much product information as possible”.
Early selection of a scalable, regulatory-friendly potency assay also enables streamlined scale-up and comparability.
As process improvements are made (for example, moving from a manual process to an automated bioreactor or changing cell expansion media), a developer can demonstrate that the product from the new process is just as potent as the old process. This comparability testing is far more convincing when supported by a validated, quantitative potency readout. Robust potency assays are fundamental not only for lot release, but also for comparability studies, process validation, and stability testing. By anchoring to an assay that regulators accept early, companies can accelerate innovation—improving their therapies and manufacturing efficiency without derailing timelines or triggering costly new clinical studies.
Another way potency assays accelerate progress is by supporting product consistency and release in clinical trials. Many cell therapies, especially autologous ones, are made fresh for each patient and have limited shelf-life. There is often urgency to release the product quickly. A well-designed potency assay can provide a timely green light for product release.
Ultimately, early potency assay strategy isn’t just about collecting more data—it’s about setting up a streamlined, compliant, and scalable development process that moves therapies to patients faster.
Custom Cell Mimics: A Strategic Enabler for Early, Reliable Potency Assays
One of the greatest barriers to developing robust potency assays early in the cell therapy process is the inconsistency of reference materials that reflect the relevant biology. This inconsistency stems from several common issues: high lot-to-lot variability during early manufacturing, difficulty qualifying target cell lines used in preclinical work, and the absence of standardized reagents that can be used across assay development and validation stages. While CAR-T cells derived from healthy donors can provide sufficient material for early-stage experiments, these sources often lack the consistency or regulatory readiness needed to support qualified assays. As a result, developers are frequently forced to delay assay development until more stable materials are available—undermining opportunities to optimize early and streamline downstream qualification.
The Alliance for Regenerative Medicine has cited the absence of standardized reference materials as a key reason for delays in assay development and regulatory approval. Without these, assay development is often delayed until sufficient primary material is available—undermining the opportunity to iterate early and optimize the process.
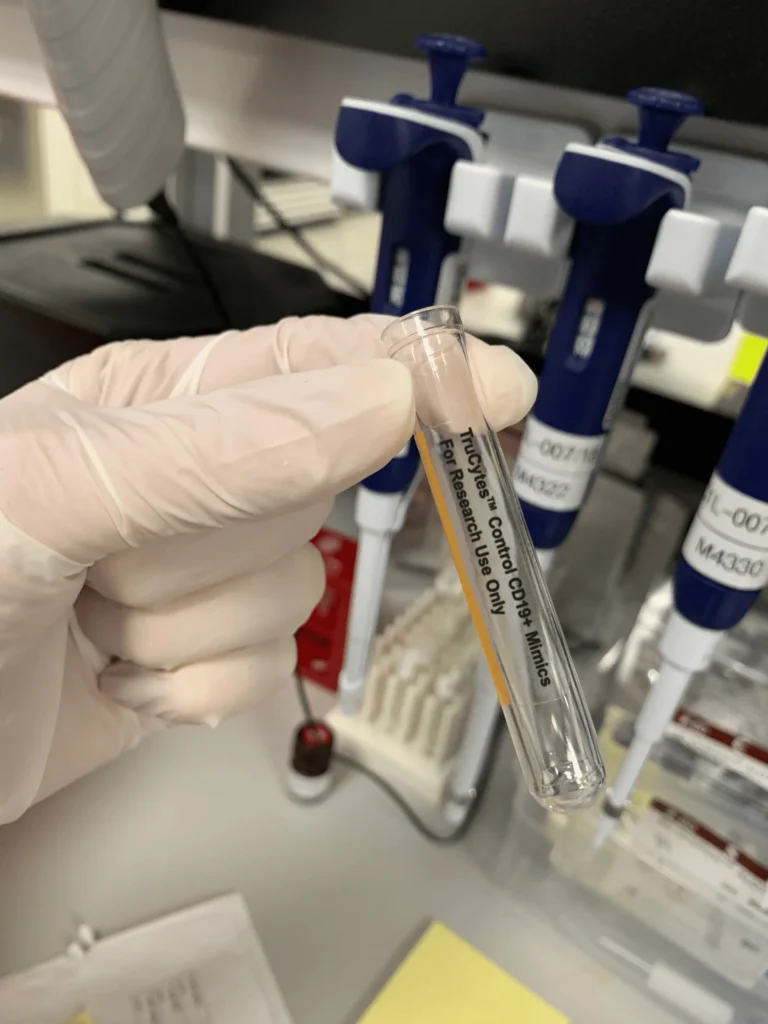
Custom cell mimic controls, such as TruCytes™, offer a compelling solution by replicating key phenotypic and functional characteristics of target cell types, including surface markers that are able to induce in vitro stimulation of the target specific CAR-T cells. These precision-engineered cell mimics enable:
- Earlier potency assay development before clinical material or final manufacturing processes are available
- Direct MoA-based functional readouts (e.g., IFN-γ secretion) that align with regulatory expectations for CAR-T potency assessment
- Standardization of assay inputs using stable, lot-matched materials to reduce variability across runs, sites, and operators
- Streamlined qualification of reagents, avoiding chain-of-custody, modification tracking, and culture maintenance challenges common to cell lines
- Flexible assay optimization, including modulation of antigen density to tune activation strength and assay sensitivity
- Reduced reliance on tumor cell lines, microbeads, or unvalidated in-house targets for regulatory-critical assay components
By integrating TruCytes or other reference tools into potency assay development, teams can design and optimize assays earlier—reducing dependency on late-phase materials and accelerating timelines for generating regulatory-ready data.
Avoiding Pitfalls and Regulatory Delays
Perhaps the strongest argument for prioritizing potency assays is the risk of development delays or failures if you don’t. Case studies abound of cell therapy programs slowed down by potency assay challenges. In fact, one analysis found that potency testing issues were cited in almost 50% of advanced therapy (ATMP) biologics marketing applications in the EU, sometimes emerging late in the review process. Imagine reaching the finish line of a Phase 3 trial only to have regulators say, “We’re not convinced your potency assay is adequate” – this scenario has forced companies to repeat studies or withdraw applications. Developing a robust assay from the start mitigates this risk. It’s far easier to refine and validate an assay during development than to solve potency questions under a regulatory clock.
A dramatic real-world example is the case of Iovance Biotherapeutics’ tumor-infiltrating lymphocyte (TIL) therapy, lifileucel. The FDA repeatedly delayed Iovance’s BLA submission and requested additional potency data because the initial single-assay approach was deemed insufficient. In 2020, FDA feedback on lifileucel’s potency assay essentially put the program on hold until a new assay strategy (a multi-assay matrix including a functional co-culture assay) was developed and validated. This led to a multi-year delay in approval. Such cases underscore that lack of an adequate potency assay can halt progress, no matter how promising the clinical results. Conversely, teams that nail down their potency assays early enjoy smoother regulatory interactions. Clear, reproducible potency data builds reviewers’ confidence that you understand your product. It can even support expedited programs – for instance, if a potency assay shows a strong correlation with clinical outcomes, it might be used to justify accelerated approval or as a surrogate endpoint in certain scenarios.
In summary, a strong potency assay strategy is not just a bureaucratic requirement; it is a potential accelerator for development. It provides the compass by which process engineers, scientists, and clinicians can navigate the complex journey of bringing a cell therapy from concept to patients. By reflecting the therapy’s true biological activity, potency assays tie together the efforts of R&D, manufacturing, and quality teams, ensuring everyone is driving toward a product that works consistently and effectively.
Key Takeaways
- Potency drives success: It’s the critical quality attribute that connects lab data to clinical outcomes—and regulators require you to measure it, lot by lot.
- Start early, move faster: Initiating potency assay development in preclinical stages helps guide process decisions, optimize outcomes, and prevent late-stage surprises.
- Solve the reference gap: Tools like custom cell mimics unlock assay development earlier—when clinical material is unreliable—by enabling consistency, reproducibility, and validation-readiness.
- Design for change: A robust potency assay enables confident scale-up, manufacturing changes, and comparability—without derailing timelines.
- Enable faster release: Short, validated potency assays allow rapid product release in trials, keeping your program on track.
- Mitigate risk: Inadequate potency strategies have stalled or sunk programs. A validated assay builds regulatory trust and can even support accelerated approval.
Potency assays serve as a driving force that aligns scientific understanding with regulatory compliance and product efficacy. By treating potency testing as a development accelerator rather than an afterthought, cell therapy teams can de-risk their programs and reach patients faster.
The investment in a robust, mechanism-of-action–relevant potency assay pays off across comparability, stability, and clinical success. As you advance your cell therapy, make potency a central pillar of your CMC strategy. Start early, iterate often, and leverage new tools – such as precision-engineered cell mimics – to enhance reproducibility, consistency, and validation.
In the next part of this series, we will delve into common challenges in potency assay development and how to overcome them. Stay tuned.